Published October 12, 2022 | BJOG: https://doi.org/10.1111/1471-0528.17321
Introduction
The United Nations reported 1.9 million stillbirths globally in 2019 with 820,000 in sub-Saharan Africa. Over 40% of stillbirths occur during labour and are preventable with high quality antenatal care and intrapartum monitoring(1). Neonatal mortality also remains high in low-income settings with a major contributor being birth asphyxia(2). Intrapartum stillbirths and birth asphyxia related neonatal deaths can be prevented with adequate intrapartum fetal monitoring and safe, expedited operative delivery when indicated.
Continuous electronic fetal monitoring (CEFM) and intermittent auscultation (IA) can both predict fetal well-being(3). In many high-income settings, CEFM has replaced IA. IA is proposed as a safe alternative to CEFM in low-risk patients with a lower rate of cesarean delivery compared to CEFM(4). Identification of low-risk patients is difficult in low-income countries due to sub-optimal antenatal care, staffing and other resource constraints. Proper IA requires a high midwife-to-patient ratio during active labour and one-on-one care during the second stage, which is also largely not achievable in low-income settings. CEFM requires equipment, knowledge, and skills that are similarly not widely accessible. Artificial Intelligence Augmented CEFM (AI-CEFM) identifies FHR abnormalities, provides a provisional interpretation, and alerts obstetric providers. AI-CEFM has potential advantages over IA and standard CEFM in settings with limited staff, lack of experience in CEFM interpretation, and a large percentage of high-risk patients.
Methods
With permission of the Malawi Ministry of Health, we instituted PeriWatch Vigilance AI-CEFM at a hospital in Malawi with over 7000 deliveries in 2021 during the height of the COVID-19 pandemic. Staff were trained on the use of the monitors, software, and identification of fetal heart rate abnormalities. AI-CEFM was employed using a risk stratification algorithm designed for staff to escalate AI-CEFM alerts to consultant level physicians.
AI-CEFM was available in four of nine labour rooms and two antenatal rooms. 24-hour obstetrician services were available for interpretation of the findings. The hospital has a 95% decision-to-delivery interval of < 30 minutes for caesarean deliveries.
Results
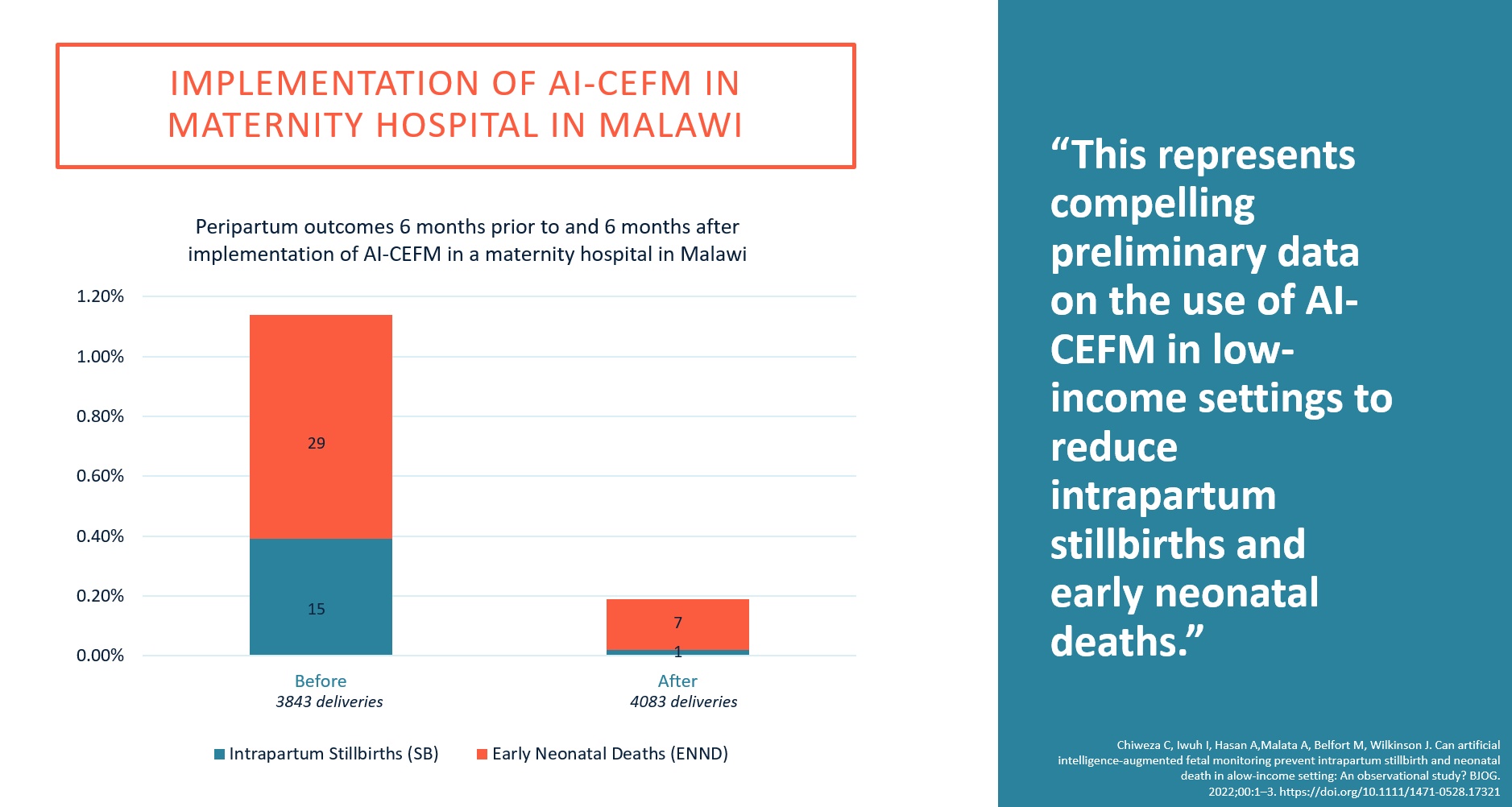
Stillbirths, early neonatal deaths and caesarean delivery rates for six months before and six months after implementation of AI-CEFM were examined. There was a marked reduction in intrapartum stillbirths and early neonatal deaths with a small but statistically significant increase in the caesarean delivery rate, as shown in Table 1.
Table 1 – Peripartum outcomes prior to and after implementation of AI-CEFM in a maternity hospital in Malawi 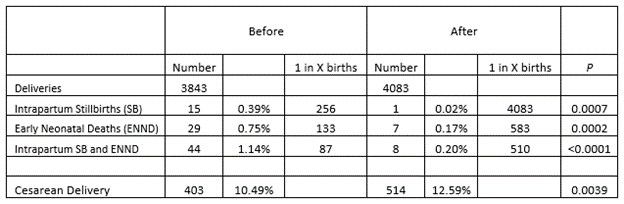
Conclusion
This represents compelling preliminary data on the use of AI-CEFM in low-income settings to reduce intrapartum stillbirths and early neonatal deaths. There are limitations in interpreting or generalizing these findings. 24-hour obstetrician coverage is not common in this setting. However, we were able to demonstrate remote interpretation of the AI-CEFM findings, emphasizing the potential for telemedicine use. This early data suggests the need for a prospective trial comparing AI-CEFM to standard CEFM and/or IA. Artificial Intelligence technology is being utilized in low-income settings for many applications. Saving babies’ lives should not be an exception.
Chiweza C, Iwuh I, Hasan A,Malata A, Belfort M, Wilkinson J. Can artificial intelligence-augmented fetal monitoring prevent intrapartum stillbirth and neonatal death in alow-income setting: An observational study? BJOG.2022;00:1–3. https://doi.org/10.1111/1471-0528.17321
References
- Danzhen You LH, Anu Mishra. A Neglected Tragedy – The global burden of stillbirths. . New York: United Nations Children’s Fund; 2020.
- Ersdal HL, Mduma E, Svensen E, Perlman J. Birth asphyxia: a major cause of early neonatal mortality in a Tanzanian rural hospital. Pediatrics. 2012;129(5):e1238-43.
- Alfirevic Z, Devane D, Gyte GM, Cuthbert A. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst Rev. 2017;2:CD006066.
- Lewis D, Downe S, Panel FIFMEC. FIGO consensus guidelines on intrapartum fetal monitoring: Intermittent auscultation. Int J Gynaecol Obstet. 2015;131(1):9-12.