Published in DotMed – Healthcare Business News
By Dr. Alana McGolrick
If you live anywhere in the United States, now is an unfamiliar time to be an expectant mother.
First, you have the high maternal morbidity rate (MMR) which affects all mothers in the U.S. That alone is cause for concern. But then there is an additional disadvantage for mothers in the 54% of rural counties that lack hospital OB units and areas where 120 rural hospitals have shut down completely over the last decade. All of which creates more pressure on the hospitals that are left while increasing inconvenience and risk for mothers and babies.
For those hospitals, implementing advanced technology that monitors mothers and babies throughout the stages of childbirth could provide support for OB nurses and physicians who are already stretched thin. The costs, however, may be beyond the budgets of small rural or critical access hospitals.
Even if they had that technology, their OB staff may be smaller than that of their more urban counterparts. And while their clinicians may be excellent, they may have less experience managing difficult labors and deliveries (L&D). As a result, rural hospital executives may elect to close their OB units rather than chance the clinical and financial risks in an increasingly litigious society.
Right now, an added complication is the COVID-19 pandemic and the complexities, emotional stress and outright fear it generates. Under normal circumstances preparing for L&D can be difficult in even the most sophisticated, well-equipped OB departments. The logistics of preparing for and maintaining a healthy pregnancy and delivery has become even more challenging when pandemic precautions are factored in. Still, the American Academy of Pediatrics (AAP) continues to emphasize that the safest place to have a baby is a hospital or accredited birthing center. The challenge is ensuring that statement is just as true for mothers and babies in rural America as it is in the largest cities.
Sharing expertise through perinatal telemonitoring
Given the unpredictability of L&D, the goal should be to ensure that quality care during childbirth is available locally. It is neither practical nor safe to expect a mother in labor to travel 100 miles (or more) to reach an OB department.
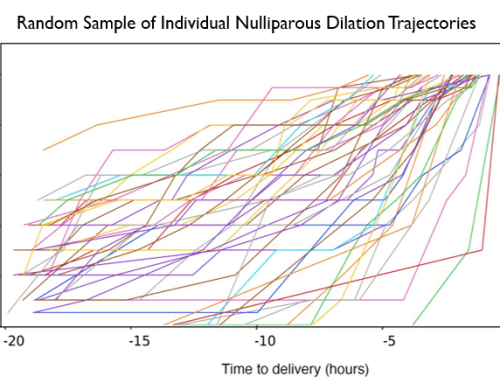
One solution that has shown early success is perinatal telemonitoring. This arrangement gives experienced OB nurses in larger urban hospitals the ability to use a central command center to monitor labor progress for mothers and babies across multiple rural settings using sophisticated, artificial intelligence (AI)-driven technologies that compare current readings to known outcomes.
Urban hospitals can then enter into agreements with rural and critical access hospitals to remotely monitor and review maternal vital sign, electronic fetal heart rate pattern and uterine activity. As a result, the smaller hospitals can relieve some of the workload from their nurses while instantly gaining access to the experience of the nurses and physicians in the large hospital.
Another significant benefit is the technology’s ability to spot negative trends as they develop. In some cases, these may just be subtle anomalies that a human might first dismiss.
When potential issues are discovered, the patients are highlighted on a color-coded dashboard. This signals the assigned registered nurses at the large hospital to investigate the reasons the patient has surfaced. The plan of care for the patient has been developed from an action plan that is agreed to by both the monitoring and monitored hospitals. Depending on the nature of the issue they can either recommend an intervention or consult with a physician and share it with nurses or physicians at the smaller hospital. By gaining this early warning, clinicians at the rural hospital can intervene before small issues become more serious.
Large hospital benefits
There are several reasons for large hospitals to participate in telemonitoring other than just the clinical help they afford to rural patients. One of the most significant is that contracting for these services with additional hospitals helps them defray some of the costs of the core solution. It can also impact the staffing costs for the remote monitoring.
The large hospital can use the perinatal telemonitoring solution to help build its obstetric service line reputation as well. Being recognized as a community leader in obstetric care will help attract highly accomplished physicians and registered nurses in high-volume markets. It can also make the hospital the preferred choice for prospective mothers over a competitor that lacks that distinction.
A monitoring hospital may also see an increase in revenue and patient volume as a result of patient referrals and transfers. In fact, a rural hospital will be more prone to transfer its high-risk L&D and neonatal patients to the large hospital with which it partners. As long as we still live in a largely fee-for-service, volume-based world, it’s important to have those relationships.
Rural hospital benefits
Besides gaining access to large hospitals’ advanced perinatal software, its IT resources and the maternal-fetal clinical expertise of its physicians and nurses, rural hospitals can realize additional benefits from telemonitoring as well. One of the most critical is they get to keep their OB department doors open so they can continue to serve their communities.
The partnership can also help rural hospitals solve staffing issues, such as fully covering the night shift and gaining access to more experienced clinicians, while remaining within budgetary limits. The lack of experienced staff can lead to assessment errors that turn into life-threatening events. With the backup of remote perinatal telemonitoring, rural hospital nurses can always seek a consultation with additional, knowledgeable colleagues about patient care during their shifts.
Better outcomes
Of course, the ultimate beneficiary is the mother-fetal dyad. Sophisticated, AI-driven technology that notifies the clinical team to negative trends early gives the team time to take action (if necessary) before the situation worsens, helping to improve patient safety and outcomes.
In a pandemic like we are currently experiencing, reducing the number of people who must physically enter rooms to check on tracings also helps protect the mother, baby and hospital staff against the spread of infectious disease.
Closing the rural/urban divide
Every American deserves nearby access to quality care, including those in rural areas. Keeping the doors to rural and critical access hospitals open, and OB departments within those hospitals, is critical to that belief.
Perinatal telemonitoring technology gives rural hospitals access to cutting-edge, AI-driven technology and expertise without the huge up-front cash outlay, enabling them to reduce clinical and financial risks while improving health outcomes. And start closing the rural/urban health divide.
About the Author: Alana McGolrick, DNP, RNC-OB, C-EFM, is Chief Nursing Officer of PeriGen, a company delivering innovative perinatal software solutions.
![]()