Multifactorial Labor Curves
Labor curves designed to improve the accuracy of predicting labor progress
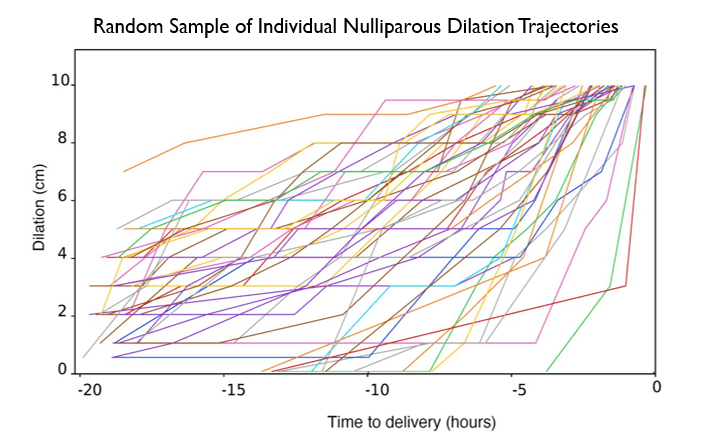
This new generation of labor curves allows for an individualized assessment of labor progress rather than a “one size fits all”
approach in a process that is naturally highly variable.
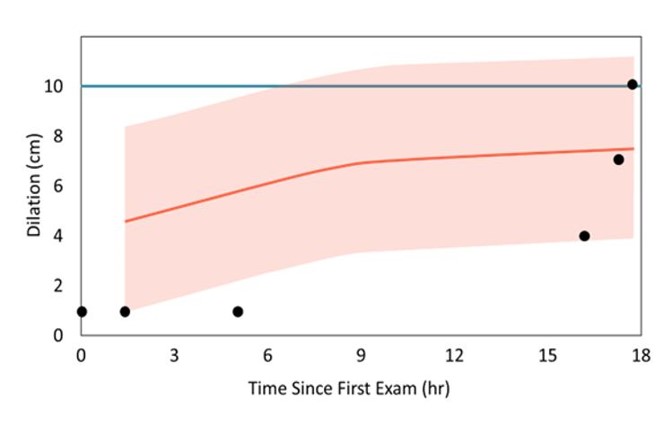
Time Alone Model
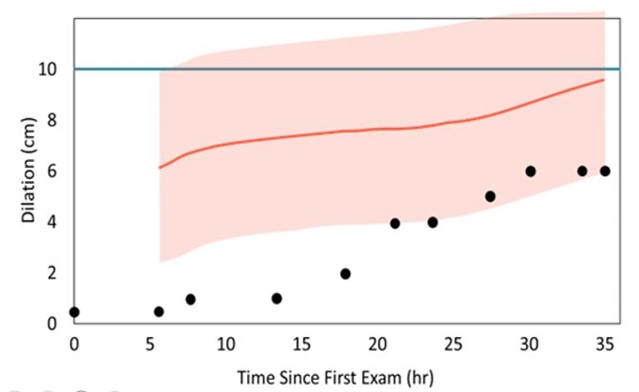
Seven Factor Model
AJOG Recognizes Study Validating PeriGen's Innovative Approach to Labor Assessment as a “Report of Major Impact”
Labor curves describe the expected course of dilation and descent in labor and in turn are used to define failure to progress, which is by far the leading case of intrapartum cesarean delivery.
The Friedman curve, first published 70 years ago, and more recent variations are based solely on the passage of time. Theses static labor curves are used by clinicians to gauge expected progress during labor.
Multifactor models mark a new generation in labor assessment. This study has shown that they are far more accurate and precise than a labor curve based solely on time, because they take into consideration several factors that affect how labor progresses.
This is the first report on the use of machine learning techniques to create labor curves of cervical dilation and fetal descent. Compared to the standard labor curve based on just the passage of time, a dilation curve based on seven clinically relevant factors has much improved accuracy and is more pertinent to clinical practice.
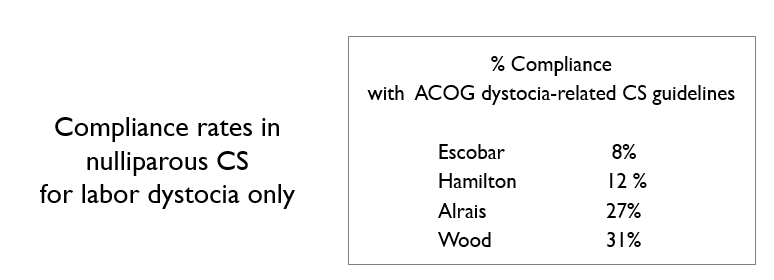
Better labor curves are needed
- low accuracy
- indifferent to the factors that directly affect dilation
- limited clinical utility
Models with multiple factors account for key factors that clinicians also consider, improved accuracy and precision, and are more responsive to labor conditions.
Why new labor curves are needed
PeriGen's Innovative Approach to Labor Assessment Validated by a Study in American Journal of Obstetrics and Gynecology
PeriGen would like to thank all of our esteemed collaborators who worked over many years through a pandemic to complete this project. Read the full article on the American Journal of Obstetrics and Gynecology.
Citation
Hamilton, E. F., Tilekbek Zhoroev, Warrick, P. A., Tarca, A. L., Garite, T. J., Caughey, A. B., Melillo, J., Prasad, M., Neilson, D., Singson, P., Mckay, K., & Romero, R. (2024). New labor curves of dilation and station to improve the accuracy of predicting labor progress. American Journal of Obstetrics and Gynecology (Print). https://doi.org/10.1016/j.ajog.2024.02.289
Authors
Emily F. HAMILTON, MD1,2, Tilekbek ZHOROEV, PhD Candidate2,3, Philip A. WARRICK, PhD2,4, Adi L. TARCA, PhD5,6,7, Thomas J. GARITE, MD8,9, Aaron B. CAUGHEY, MD, PhD10, Jason MELILLO, MD11, Mona PRASAD, DO, MPH12, Duncan NEILSON, MD13, Peter SINGSON, MD13, Kimberlee MCKAY, MD2,14,15, Roberto ROMERO, MD, DMedSci16,17,18
Affiliations
1Department of Obstetrics and Gynecology, Faculty of Medicine and Health Sciences, McGill University, Montreal, QC, Canada
2PeriGen Inc., Cary, NC
3Department of Applied Mathematics, Faculty of Science, North Carolina State University, Raleigh, NC
4Department of Biomedical Engineering, Faculty of Medicine and Health Sciences, McGill University, Montreal, QC, Canada
5Center for Molecular Medicine and Genetics, Wayne State University, Detroit, MI
6Department of Obstetrics and Gynecology, Wayne State University School of Medicine, Detroit, MI
7Department of Computer Science, Wayne State University College of Engineering, Detroit, MI.
8E.J. Quilligan Professor Emeritus, Obstetrics and Gynecology, University of California, Irvine, Irvine CA
9Senior Vice President of Clinical Sciences, Sera Prognostics: The Pregnancy Company, Salt Lake City, UT
10Department of Obstetrics and Gynecology, Oregon Health & Science University School of Medicine, Portland, OR
11Obstetrics and Gynecology, OhioHealth, Columbus, OH
12Maternal-Fetal Medicine, OhioHealth, Columbus, OH
13Women’s Health Services, Legacy Health, Portland, OR
14Sanford School of Medicine at the University of South Dakota, Vermillion, SD
15Perinatal Quality and OB/GYN Service Line, Avera Health, Sioux Falls, SD
16Pregnancy Research Branch, Division of Obstetrics and Maternal-Fetal Medicine, Division of Intramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, US Department of Health and Human Services, Bethesda, MD
17Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor, MI
18Department of Epidemiology and Biostatistics, Michigan State University, East Lansing, MI