As the relationship between informatics and healthcare has evolved, a delicate technical and clinical decision-making balance has developed. This balance encompasses the patient’s individual clinical picture, the clinician’s assessment, and the influence of technology on healthcare decision-making (Mastrian & McGonigle, 2017). Utilization of healthcare informatics tools and clinical decision support systems has shown to have positive effects on patient care outcomes, while improving efficiency of care delivery (Lee, 2013; Mastrian & McGonigle, 2017). With the emergence of new informatics tools in healthcare, the clinician should be well-versed in information sciences, its patient-specific application, and impact to their practice. An exciting product in healthcare informatics includes computerized clinical decision support systems (CCDS). CCDS can be found in several formats, such as diagnostic algorithms or rules-based alerts and can be embedded in electronic health records etc. (Lytle, Short, Richesson & Horvath, 2015).
Artificial intelligence (AI) is another technique in some CCDS. AI or more specifically neural network techniques, use sophisticated mathematical processes to “learn” the association between specific patterns in patient information and a specific outcome. (Alexander, 2006). Once the training process is complete, the trained neural network unit can be embedded in a CCDS module to search for the specific patterns it had learned to be associated with that outcome. Nonmedical examples of AI-based pattern recognition are found in voice recognition in phones, face recognition in cameras and in robots that play chess. In medicine, AI systems assist a wide variety of problems from cancer diagnosis on radiological images or cytology preparations and to sepsis prediction in the ICU.
In medicine, CCDS are designed to augment existing data systems to assist the healthcare clinician with decision-making regarding patient care (Alexander, 2006; The Office of the National Coordinator of Health Information Technology, 2017). CCDS may be triggered by certain collections of words within the EMR or particular pharmacy selections or data from patient monitors or a combination of all of the above.
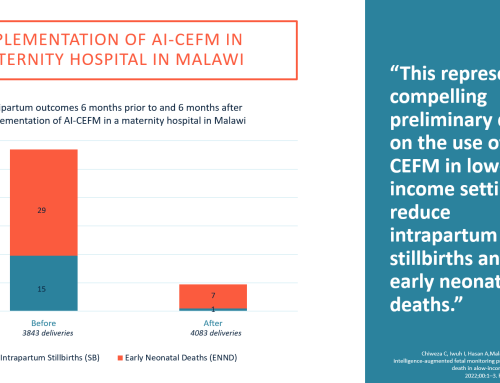
CCDS can alert the clinician that the patient is within the desired and established patient specific norms, and most importantly, if the patient breaches preset physiological parameters. Fetal heart rate pattern recognition software is an example of a neural network that has learned to identify specific fetal heart rate patterns, for example accelerations, contractions and types decelerations (Warrick, Hamilton, & Macieszczak (2005). By recognizing these events, the software is able to alert the staff to worrisome combinations such as uterine tachysystole or recurrent late decelerations. These alerts notify the clinician that the patient’s situation requires additional assessment, intervention and/or escalation of care. The use of CCDS does not negate clinician judgment but strengthens the clinician’s interpretation of the data and provides justification for the chosen care plan. By providing the clinicians with alerts, the CCDS can enhance decision-making, improve communication and potentially impact patient outcomes (The Office of the National Coordinator of Health Information Technology, 2017).
As information technology becomes even further integrated into all aspects of healthcare, patient safety and quality of care will benefit greatly. By utilizing data readily available in electronic health records or via patient monitoring systems, clinicians can objectively assess patient data. Support from the CCDS will provide value and long-term benefits to the patient and healthcare organization. These benefits include the potential to avert serious clinical events, and improved patient and provider satisfaction.
References
Alexander, G. L. (2006). Issues of trust and ethics in computerized clinical devsion support systems. Nursing Administration Quarterly, 30(1), 21-29. doi:
Hunt, D. L., Haynes, B., Hanna, S. E., & Smith, K. (1998). Effects of computer-bases clinical decision support systems on physician performance and patient outcomes: A systematic review. Journal of Americal Medical Association, 280(15), 1339-0000. doi:
Lee, S. (2013). Features of computerized clinical decsion support systems supportive of nursing practice: A literature review. Computers, Informatics, Nursing, (31(10), 477-495. doi:
Lytle, K. S., Short, N. M., Richesson, R. L., & Horvath, M. M. (2015). Clinical decsion support for nurses: A fall risk and prevention example. Computeres, Informatics, Nursing, 33(12), 530-537. doi:
Mastrian, K., & McGonigle, D. (2017). Patient engagement and connected health. In McGonigle, D. & Mastrian, K. (2017). Nursing informatics and the foundation of knowledge (4th ed., pp. 237-262). Burlington, MA: Jones& Bartlett.
Staub-Muller, M., de Graaf-Waar, H., & Paans, W. (2016). An internationally consented standard for nursing process-clinical decision support systems in electronic health records. Computers, Informatics, Nursing, 34(11), 493-502. doi:
The Office of the National Coordinator of Health Information Technology https://www.healthit.gov/
Warrick, P., Hamilton, E., & Macieszczak, M. (2005). Neural network based detection of fetal heart rate patterns. In Neural Networks, 2005. Proceeding. 2005 IEEE International Joint Conference, 4, 2400-2405.
Weber, S. (2007). A qualiative analysis of how advanced practice nurses use clinical devision support systems. Journal of American Academy of Nurse Practioners, 19(12), 652-667. doi:10.1111/j.1745-7599.2007.00266.x