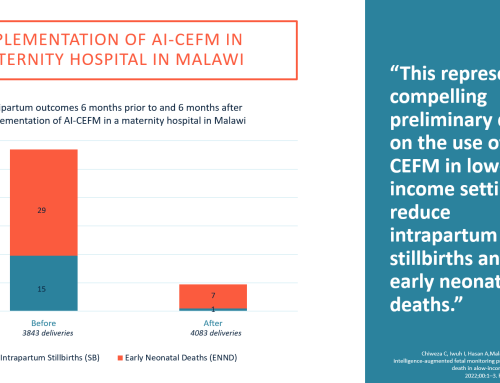
Machine learning supplements electronic fetal monitoring to help improve clinical efficiency, timely intervention, and standardization of care.
By Dr. Emily Hamilton, MDCM – Senior Vice President of Clinical Research, PeriGen
Electronic Fetal Monitoring (EFM) has been a foundational technology in perinatal obstetrics since the 1970s for recognizing fetal distress during labor. While the technology has changed little in the ensuing years, the demands on providers and coordinators of labor and delivery (L&D) care––perinatal nurses––have intensified. Meanwhile, a new class of EFM technologies are emerging and enabling new levels of monitoring capabilities and, in turn, safety for expectant mothers and their babies.
In recent years, artificial intelligence (“AI,” and in particular, machine learning), has gained traction throughout medicine, and is now used to enhance fetal and maternal safety in L&D. There are already numerous machine learning applications throughout medicine that perform pattern recognition––interpreting x-rays, for example. The technology is now being applied to patients in L&D. Machine learning provides consistent, objective, data-driven analysis that can not only complement human abilities, but also help compensate for potential lapses related to fatigue, stress, inexperience, and the well-documented nursing shortage.
Interpreting Labor-Induced Stress
The process of labor initiates a host of stresses on the unborn baby in the form of contractions, which induce transient declines in oxygen delivery, and movement through a narrow passage. All babies experience a degree of oxygen deprivation (hypoxia) during contractions. However, this is typically mild and tolerated well. When it is prolonged, excessive, or if the baby is not equipped to deal with it, the resulting injury can be devastating––even deadly.
While hypoxia-related injury rates in the United States are among the lowest in the developed world, studies reveal that half or more of these poor outcomes (most related to issues around fetal heart rate monitoring) are preventable. This situation is not unique to the United States. Studies conducted throughout the Western world have drawn the same conclusion. Meanwhile, approximately one-third of women in the U.S. deliver babies by cesarean section, which is surgery with associated risks. And among first-time mothers, about half of these procedures are related to fetal heart rate patterns, with much of the other half linked to slow labor progress.
Most preventable hypoxic injuries track back to human interpretation of fetal heart rate tracings. So why do we rely on fetal heart rate tracings to assess fetal status? Because the fetus is mostly inaccessible during birth and its heart rate is the only measurement that is practically available throughout labor. Interpretation of fetal heart rate tracings remains a problem for clinicians who work under demanding conditions.
There are certain patterns in a fetal heart rate that indicate a baby is not tolerating labor well, but it’s not a simple one-to-one relationship. A myriad of patterns, combinations, and trends over time must be evaluated. It is up to the clinician to put this all into context incorporating other factors known about the patient. It is, admittedly, an imperfect science.
Maternal Monitoring and Labor Progression
Fetal heart rate pattern analysis is fundamental in evaluating a baby’s tolerance of labor. But assessments of labor progress––verifying if the baby is descending and if the uterus is dilating as it should, ––are also important.
Nurses periodically measure the mother’s blood pressure, pulse, respiratory rate, and a few other indicators. Some of these are sensors, others are measured and recorded manually. Assessing a mother’s status regarding progress of labor is an imprecise science. There are many factors to consider, and even if all factors are weighed, no two mothers respond in the same way. Assessment of a complicated process is another problem that can be standardized using mathematical techniques.
Given the range of variables to consider in monitoring the wellbeing of both babies and mothers, we increasingly rely on computers to analyze complex situations reliably, and quantitatively, rather than qualitatively.
Supplementing Clinicians With a “Second Set of Eyes”
L&D nurses must examine and document a range of 5 to 10 unique characteristics in each tracing every 15 to 30 minutes, depending on the stage of labor. Some of these measures are simple, such as counting the number of contractions a patient has had in the past 10 or 30 minutes. Still, employing a highly skilled nurse to count contractions is not a good use of time or resources.
It’s no secret that L&D clinicians work under difficult circumstances. Long hours, with peak activity often in the middle of the night, when judgment may not be at its best. Then factor in caring for multiple patients at the same time and the clinician’s experience level (another factor exacerbated by pandemic-induced attrition). The current nursing shortage has necessitated extraordinary working hours, and nurses are exhausted and are being pulled in from other units to address the crisis and ensure coverage.
L&D nurses can easily analyze fetal heart rate tracings, but doing so consistently, efficiently, helping the inexperienced nurse, or the float who’s brought in from another unit remain challenges. These very real situations pose a substantial risk for patients.
This is where AI-powered technology is emerging as a consistent method to help analyze tracings and other crucial measurements over time.
Pattern Recognition and Data Consolidation
Consider a computerized system, not affected by fatigue or emotion, or patient load, which can bring the interpretation of fetal heart rate patterns to a high, consistent, and standard level. This is where new applications powered by machine learning algorithms represent a much-needed “extra set of eyes” to monitor both the condition of the unborn child and the labor progression of the mother.
Machine learning is ideal for pattern recognition in fetal heart rate recordings because it is a type of mathematics that can deal with variation in presentation. Consider the variations in handwriting––no one signs their name the exact same way twice, yet AI applications can recognize signatures despite slight variations. Fetal heart rate patterns are also variable but far more complex––because are examined in the context of a noisy background. In addition, they must be examined for how they evolve over time.
Machine learning is now applied to recognize, detect, label, and measure these fetal heart rate patterns. Some L&D monitoring systems can consolidate up to 12 hours of data on a single screen with color-coding to highlight results that exceed safety norms set by the hospital. Nurses and obstetricians can then refer to this highly visual dashboard to rapidly evaluate trends, including the state of both mother and fetus and the progression of labor.
Being able to visualize the trends in the fetal heart rate patterns, maternal vital signs, and labor over time provides a more complete picture, compared to stitching together disjointed snapshots.
Aside from driving standardization, precision, and consistency, these machine learning-powered applications for L&D represent a substantial labor saver for nurses who must document their findings, and then consolidate and synthesize that collective data into decisions and action.
And because new nurses do not feel as alone, and know they have back-up, this capability helps administrators in their recruiting efforts. It also enables more virtual monitoring, such as what occurred during the pandemic, when some bedside nurses were unable to work in the department because of their own health conditions or risks of viral exposure. AI-based monitoring systems empowered these nurses to oversee tracings remotely, allowing them to support the bedside team from 20 feet or 20 miles away.
This technology works seamlessly alongside existing perinatal systems, adding automated early warning capabilities to help clinicians flag concerning trends in patients’ status. It is a good example of combining the best of two worlds: technology consolidates and trends data, analyzes, and highlights deviations from expected norms – while clinicians apply their in-depth knowledge and judgment to make well-informed decisions and take timely actions.