Video Transcript: Introduction to Early Warning Systems
Welcome to early warning systems for labor and delivery.
This video covers the types of early warning systems, their impact, and the research associated with them. We also look at an automated option for early warning systems used in labor and delivery. Our featured presenter is Emily Hamilton, senior vice president of clinical research at PeriGen. Emily is widely published, presents often at obstetric conference,s and is an adjunct professor of obstetrics at McGill University.
Emily: Welcome everybody.
Let’s begin with a definition. There are two fundamental components to early warning systems. There is a set of alert criteria which are usually based on vital signs plus or minus other features and they are designed to prompt clinical action. The IHI calls them scorecards that save lives and early warning systems are present in a variety of medical specialties.
How do they work?
Assessments are made routinely and repeated periodically and, when there is an abnormality, the results are tied to specific actions which may be a physician assessment at the bedside, calling a rapid response team, or initiating a specific set of investigation therapy or actions. Let’s go back to history. Early warning systems were initiated in the UK in 2007. The report from the confidential inquiries on maternal deaths made a recommendation that all OB units adopt an early warning system for all obstetric or patients and in the ensuing five years you can see that there was a great increase in the use of obstetrical warning systems in the UK.
Now let’s turn to some experience in the United States. There are two statistics which are very striking. One relates to infant mortality. The US ranks number five in high rates of infant mortality among the 35 countries of the OECD. Maternal mortality rates are also disturbing. Not only is the US rated higher than all of the high-income countries listed here, its rates are rising whereas the others are falling. There are regional exceptions. As shown here, mortality rates in California, in blue, have been falling steadily since 2008. We have much to learn from California.
This study is an examination of 207 maternal mortality cases from California and you could see here the leading causes. Cardiovascular disease the most frequent. A detailed review regarding causes and opportunities for improvement concluded that 41% had a strong chance for prevention and another 48% had some chance to alter outcome with different care. So even in California, with excellent maternal mortality rates and trends, a high percentage of those are preventable.
Well, let’s look at early warning systems in more detail. As mentioned before, they’re designed to identify patients who are developing serious acute illness and to prompt timely response. There are many variations and many acronyms as you can see here and we will look at three in particular.
The National Partnership for maternal safety includes representatives from 21 professional organizations in the United States. They met to find a simple early warning system with the acronym MEWC. The criteria are 7. I’ve listed them here. If any one of these thresholds is exceeded, it initiates prompt bedside evaluation and activation of resources to initiate emergency interventions as necessary.
Now, MEOWS is the early warning system that was developed in the UK. It includes eleven items and each item is scored from zero to three based on the degree of abnormality. Once the eleven factors have been scored, the total MEOWS score is a sum of all of the individual scores. Paper charts are color-coded to facilitate the scoring and you can see on the right that this is quite an extensive procedure with frequent multiple facets being scored and the total score recorded in the bottom level with the purple banner. Depending upon the score, different clinical actions are activated. To say the least, this is a very labor-intensive process, but as you saw earlier UK was one of the countries where rates of maternal mortality are consistently falling.
The next one that we’re going to look at is MEWT. The ‘T’ stands for trigger and this is the one used in the Californian studies that I’m going to describe in a few minutes. It has seven features and this time the blood pressure features require, in addition to being above or below a certain threshold, a degree of persistence. This was introduced to reduce trivial alarms related to transient and non-persistent abnormalities in blood pressure. This is the action items that are tied to the MEWT system.
Clinical Impact
Next, let’s look at some clinical impact using this system. This is a large study. It involves close to 70,000 patients in 23 hospitals. It’s a before and after study. As you can see, the rate of correct anti-hypertensive treatment went from 57 to 90% and the rate of correct magnesium sulfate utilization went from 85 to 96%. With better care, it’s not surprising to see better outcomes and indeed in eclampsia rates fell from 1.15 to 0.62 per thousand births. Severe maternal morbidity, as defined by the CDC definitions (so very severe maternal morbidity) went from 2.4 to 2.0 percent.
Causes of Medical Error
I’d like to spend a couple of minutes talking about causes of medical error. We’re very familiar with causes of medical conditions or medical illness. That’s what directs our diagnosis and our treatment. So, understanding the causes of medical error is important because it helps to identify what are the mitigation strategies that are most likely to be successful. This is a
study which involves an analysis of different causes of medical error in two conditions very near to our hearts in obstetrics. On the left, neonatal encephalopathy and on the right maternal mortality. At the top, in black, is the relative proportion that was related to lack of knowledge or skills. Deficiencies and knowledge or skills are important. They must be urgently addressed and that’s the role of traditional education, credentialing, simulations, certifications.
You can see that the majority of the errors related to clinician factors were not lack of knowledge or skills but were more related to judgment. How we think about a problem. The bottom stippled red block represents failure to recognize the severity or complexity of a problem. Above that, the portion related to miscommunication. Above that, failure to seek help. And the last one, delayed response.
Another name for this collection of problems is poor situational awareness.
What is situational awareness? It is the ability to determine where my patient is in the spectrum of normal to highly abnormal and to project what’s about to happen. If I can do that well, then it’s likely I will institute prompt and appropriate clinical actions. There are several well defined steps that are necessary for good situational awareness. First, we have to have all the relevant data. Two, we have to understand what it means. Three, we must project what is about to happen. This is particularly critical in obstetrics because not only do we have a maternal condition to be concerned about and a fetal condition, but they’re very much related to labor and the labor ends often stresses on the mother and the baby well resolved. So not only do we have to project what’s happening to our mother and baby, but what’s happening to the labor. Finally we have to act, which of course requires that we have the appropriate skills and access to equipment and medications etc. All of these steps are essential to arrive at the correct action. The blue squares represent complex reasoning – things that we are taught in our professional training and learn with experience. The yellow squares are things where computers can help.
Introduction to PeriWatch® Vigilance™
 Now, I’d like to show you what we can do to help in this process. Before I show you these screens, this product is in development. It is called PeriWatch Vigilance and this is only a preview. The software is under development and the screens which I’m going to show you our artistic renditions. They will certainly change.
Now, I’d like to show you what we can do to help in this process. Before I show you these screens, this product is in development. It is called PeriWatch Vigilance and this is only a preview. The software is under development and the screens which I’m going to show you our artistic renditions. They will certainly change.
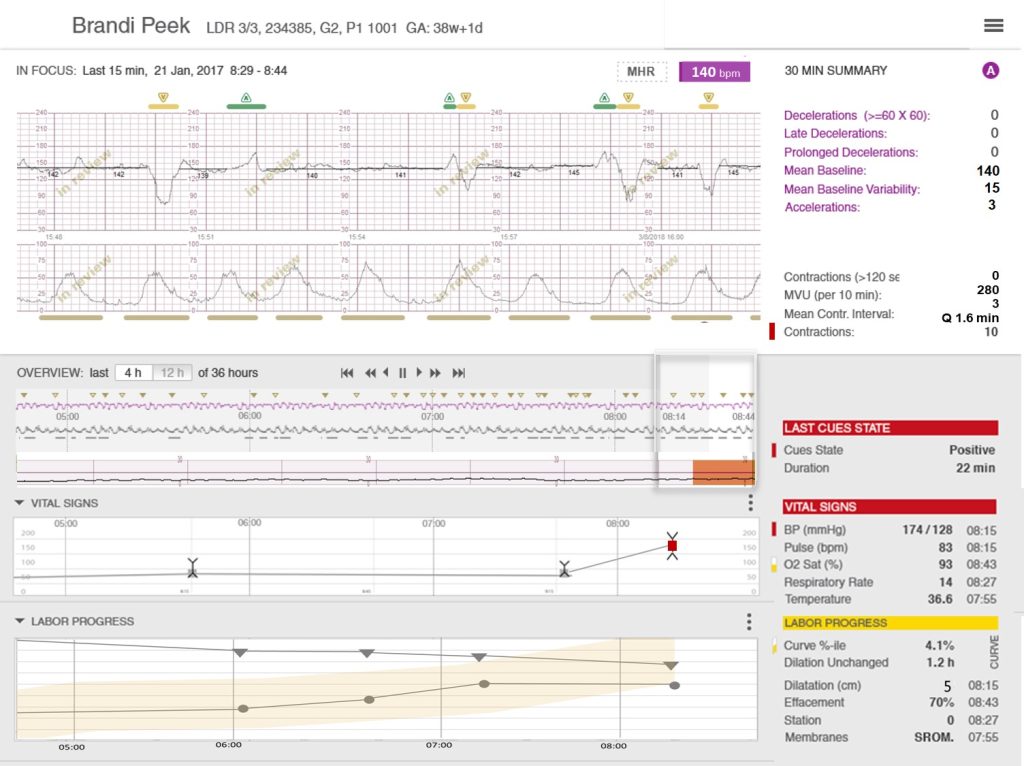
To begin with, you see some things that are familiar: A detailed portion of the tracing on the top, underneath a compressed view of the tracing which can span either four or twelve hours. This movable slider window will select any portion and a compressed view for details. Now, however, you can choose to view either 15 or 30 minutes. Here we’re looking at 15 minutes. Beneath the compressed view is a color-coded bar which show us in orange when any of that tracing above hasn’t met any one of the six HCA oxytocin checklist criteria. Finally up on the right is a series of measurements that pertain to the tracing enclosed by that movable window. To the right of the compressed view is a panel which tells the most recent state according to the classification you have chosen and it will highlight which feature has caused it to be triggered into that condition.
Below the tracing are two more interactive panels. The first one relates to vital signs and by clicking on that you can open it and see the vital signs for the last four hours (if you have chosen a four-hour compressed view or twelve hours if that has been chosen). Again, the vital signs which exceed certain thresholds set by your institution are color-coded sort so it’s easy for you to identify what has caused the vital signs panel to turn a particular color. Beneath that is the labor progress view, important because of the implication of duration of labor on maternal and fetal condition. These are collapsible, however their current state will remain color-coded so even without opening them you can see whether or not there is something of concern.
In conclusion, regarding early warning systems, we see that there is widespread use across many domains in medicine. There has been wide adoption in UK maternity units of the obstetrical variations. MEWT, one that has been developed in California, is associated with clinical improvement in leading US centers and they are all fairly work intensive. Parts of the early warning system process are well-suited for computerization. Computers are tireless. Not subject to vigilance fatigue. And good at organizing and displaying complex data. Cinicians are intelligent, skillful, empathetic, hard-working. These two different assets make for a very powerful combination.
Thank you very much for joining us for this introduction to early warning systems.
