The importance of longer EFM views
 by Emily Hamilton, MD CM
by Emily Hamilton, MD CM
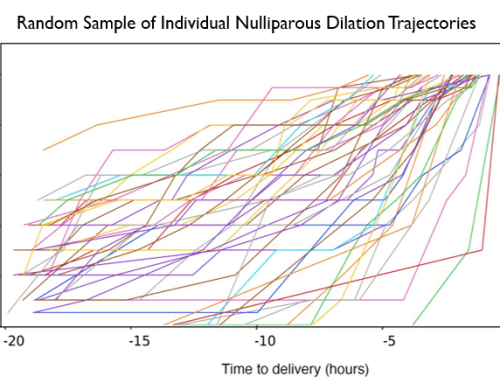
Senior Vice President, Clinical Research
Labor and delivery clinicians use EFM to identify fetal intolerance to labor to guide intervention and prevent hypoxic fetal injury. This task requires not only assessing the past and current degree of tracing abnormality and but projecting what is likely to happen in the near future. There is good evidence that tracing abnormalities generally evolve over hours (1-3). In addition, intervention guidelines usually recommend evaluating fetal response to supportive interventions over 30 to 60 minutes before resorting to cesarean delivery (4, 5). Thus long term assessments are essential. Standard computerized displays provide views of only 8 -10 minutes of tracing. Short term “snapshot” views can contribute to a failure to appreciate duration of tracing abnormality and the likely evolution.
PeriCALM Checklist analyzes EFM tracings in a consistent fashion. Its displays show long term trends over several hours, color coding regions of abnormality according to the criteria set by the institution. Such displays help clinicians see if a problem is intermittent or persistent, improving or deteriorating, stable or changing rapidly. A view of EFM trends may assist with situational awareness and helps clinicians in acute care settings more accurately project what is likely to happen and institute appropriate care. Checklist techniques and methods are especially pertinent in acute care settings during night time work when large amounts of data must be processed by the care givers over many hours. (6,7)
1. Vintzileos AM, Smulian JC. Decelerations, tachycardia, and decreased variability: have we overlooked the significance of longitudinal fetal heart rate changes for detecting intrapartum fetal hypoxia? Am J Obstet Gynecol. 2016 Sep;215(3):261-4.
2. Elliott C, Warrick PA, Graham E, Hamilton EF. Graded classification of fetal heart rate tracings: association with neonatal metabolic acidosis and neurologic morbidity. Am J Obstet Gynecol. 2010 Mar;202(3):258.
3. Clark SL, Hamilton EF, Garite TJ, Timmins A, Warrick PA, Smith S. The limits of electronic fetal heart rate monitoring in the prevention of neonatal metabolic acidemia. Am J Obstet Gynecol. 2016 Oct 14. pii: S0002-9378(16)30872-9. doi: 10.1016/j.ajog.2016.10.009. [Epub ahead of print]
4. Clark SL, Nageotte MP, Garite TJ, Freeman RK, Miller DA, Simpson KR, Belfort MA, Dildy GA, Parer JT, Berkowitz RL, D’Alton M, Rouse DJ, Gilstrap LC, Vintzileos AM, van Dorsten JP, Boehm FH, Miller LA, Hankins GD. Intrapartum management of category II fetal heart rate tracings: towards standardization of care. Am J Obstet Gynecol. 2013 Aug;209(2):89-97.
5. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009 Jul;114(1):192-202.
6. Chapter 46. Fatigue, Sleepiness, and Medical Errors. AHRQ. (accessed December 2, 2016) https://archive.ahrq.gov/clinic/ptsafety/chap46a.htm
7. Fioratou E, Flin R, Glavin R, Patey R. Beyond monitoring: distributed situation awareness in anaesthesia. Br J Anaesth. 2010;105:83-90.