The following excerpt summarizing the factors regulating the fetal heart rate will be summarized in the free March 16th lunchtime L&D staff training webinar titled “The Physiology of EFM” featuring Emily Hamilton, MDCM.
What Regulates the Fetal Heart Rate?
The heart is a muscle with its own pacemaker, conducting system, numerous types of receptors (alpha and beta adrenergic) and direct neuronal connections to both the sympathetic and parasympathetic systems.
The overarching mission of the cardiovascular system is to deliver sufficient oxygen to key organs. Heart rate is an important determinant of this mission.
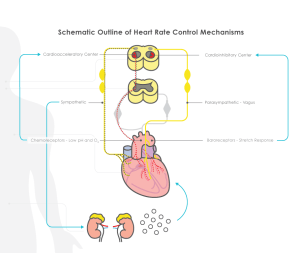
Ultimately, any influence on heart rate is mediated by one or more of these structures. The basic anatomy and physiology of heart rate control are described in physiology textbooks. In the simple schematic diagram shown in Figure 1, factors which increase heart rate are shown on the left and factors which decrease heart rate are on the right. While this summary provides the basics for understanding heart rate regulation, it is important to remember that our understanding of this physiology continues to evolve.
The cardioregulatory center in the medulla oblongata contains an acceleratory center and an inhibitory center. The cardioregulatory center receives input from the central nervous system, reflex pathways and circulating catecholamines. An example of central nervous system influence on the acceleratory response is seen with vibroacoustic stimulation. In response to sudden auditory stimulation, the central nervous system activates the cardioacceleratory center. The cardioacceleratory center increases heart rate directly via sympathetic cardiac nerves which interact with the sinoatrial node to increase the heart rate.
The rapidity of heart rate change is determined by the conditions that trigger the change.
The cardioinhibitory center slows the heart rate via the parasympathetic vagus nerve which can slow heart rate by modulation at various levels, including the sinoatrial node. Reducing cardioinhibitory activity increases heart rate.
Arterial baroreceptors, located in the aortic arch and carotid arteries, are sensitive to stretch or distension of a vessel caused by blood pressure changes. An increase in arterial blood pressure produces vessel distension and causes arterial baroreceptors to send neuronal messages to the cardioinhibitory center, which in turn causes rapid slowing of the fetal heart rate via the parasympathetic vagus nerve. A decrease in arterial pressure results in an increased heart rate.
Arterial chemoreceptors located in the aortic arch and carotid arteries are sensitive to low pH and low oxygen saturation. When these chemoreceptors are activated, they cause the cardioacceleratory center to increase sympathetic impulses, resulting in an increase in the fetal heart rate. The α-adrenergic component of the chemoreceptor response causes vasoconstriction and hypertension. As will be described later, hypertension is an important part of the pathway producing fetal heart rate decelerations.
The catecholamines, epinephrine and norepinephrine, secreted from the adrenal, are both hormones and neurotransmitters. Norepinephrine binds to beta receptors in the heart causing an increase in heart rate, contractility and stroke volume. Catecholamines can also cause redistribution of blood flow by inducing vasoconstriction and vasodilation in different regions. Vasoconstriction is mediated through the α-adrenergic receptors in liver, kidney, skin and gut, and vasodilation is mediated through β adrenergic receptors in skeletal muscle. Catecholamine release is stimulated by the sympathetic nervous system and may be precipitated by stress conditions, such as loud sounds, fear or low blood sugar.
The rapidity of heart rate change is determined by the conditions that trigger the change. Central stimuli like a sudden loud sound or a quick increase in blood pressure cause rapid heart rate changes mediated by direct neuronal pathways to the sinoatrial node. Although chemoreceptor action on heart rate is also mediated neuronally (by the cardiac nerves), this influence tends to be slow because it is triggered by low pH and oxygen levels which tend to fluctuate slowly. Catecholamine mediated effects are relatively slow reflecting their half-life of 2 to 3 minutes.
While all of the mechanisms described above modulate heart rate, it is important to recall that the overarching mission of the cardiovascular system is to deliver sufficient oxygen to key organs. Heart rate is an important determinant of this mission but only one, along with other cardiovascular compensatory mechanisms, which include redistribution of blood flow and changes in blood pressure, cardiac stroke volume or oxygen carrying capacity and hemoglobin-oxygen dissociation in the blood stream. The medulla oblongata contains the vasomotor center that responds to baroreceptors, chemoreceptors and catecholamines. It also regulates peripheral blood vessel dilation and constriction to help maintain normal blood pressure and distribution of blood to vital organs.