The “cat’s whiskers” behind a
key concept of obstetrical safety
by Emily Hamilton, MD CM
No, we have not taken to caring for cats or declining Latin verbs. Yes, we are “over the top” on the concepts behind these acronyms and their contributions to obstetrical safety. MEWS1,MEWT2, MEOWS3 refer to examples of Maternal Early Warning Systems that operate in addition to usual clinical care. They have been proposed to facilitate timely recognition, diagnosis and treatment of patients developing critical illness. This assistance is relevant today because delayed recognition and intervention remain contributory factors in about half of births with maternal deaths or neonatal encephalopathy.4, 5
MEWS, MEWT and MEOWS are scoring systems based on a short checklist of key criteria,
 primarily vital signs. Some variants add factors such as persistence, level of consciousness, urine output, lab tests or fetal condition. Some use color coding or weighting for different levels of abnormality. Important characteristics of successful warning systems are:
primarily vital signs. Some variants add factors such as persistence, level of consciousness, urine output, lab tests or fetal condition. Some use color coding or weighting for different levels of abnormality. Important characteristics of successful warning systems are:
- Assessments are routine and repeated periodically, e.g. on admission and at frequent intervals
- Specific scores are tied to specific actions e.g. physician assessment, calling a rapid response team or initiating a specific investigation or therapy.
In obstetrics, early warning scores on ICU admission were strongly related to maternal mortality.6 A large “Before and After” study in the US found very significant reductions in severe maternal morbidity in the group where an early warning system was implemented and no changes in these rates in the control group without a warning system.7 A survey of 130 maternity units in 2013 in the UK indicated that 100% had implemented a formal early warning system, up from 19% in 2007.8
We are still learning the impact of Early Warning Systems in obstetrics and how to optimize them to improve efficiency. Nursing effort and alarm fatigue are important considerations.
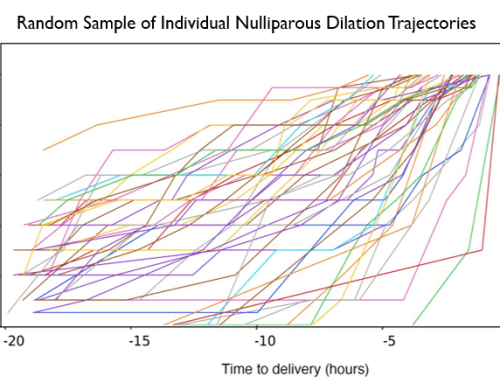
But wait…. software could reduce that nursing effort by using information already recorded in the electronic medical record. In addition it could track how often and how early a particular trigger appears. We could use statistical techniques to determine exactly what clusters of parameters are most useful.
Stay tuned … the best is yet to come. Look for more information on this topic later this year.
References
1 Mhyre JM, DʼOria R, Hameed AB, Lappen JR, Holley SL, Hunter SK, Jones RL, King JC, DʼAlton ME. The maternal early warning criteria: a proposal from the national partnership for maternal safety. Obstet Gynecol. 2014 Oct;124(4):782-6.
2 Hedriana HL, Wiesner S, Downs BG, Pelletreau B, Shields LE.
Baseline assessment of a hospital-specific early warning trigger system for reducing maternal morbidity. Int J Gynaecol Obstet. 2016 Mar;132(3):337-41.
3 Singh S , McGlennan A, England A, Simons R. A validation study of the CEMACH recommended modified early obstetric warning system (MEOWS). Anaesthesia. 2012 Jan;67(1):12-8.
4 Main EK, McCain CL, Morton CH, Holtby S, Lawton ES. Pregnancy-related mortality in California: causes, characteristics, and improvement opportunities. Obstet Gynecol. 2015 Apr;125(4):938-47.
5 Sadler LC, Farquhar CM, Masson VL, Battin MR. Contributory factors and potentially avoidable neonatal encephalopathy associated with perinatal asphyxia. Am J Obstet Gynecol. 2016 Jun;214(6):747.e1-8.
6 Carle C, Alexander P, Columb M, Johal J. Design and internal validation of an obstetric early warning score: secondary analysis of the Intensive Care National Audit and Research Centre Case Mix Programme database. Anaesthesia. 2013 Apr;68(4):354-67.
7 Shields LE, Wiesner S, Klein C, Pelletreau B, Hedriana HL. Use of Maternal Early Warning Trigger tool reduces maternal morbidity. Am J Obstet Gynecol. 2016 Apr;214(4):527.e1-6.
8 Isaacs, RA, Wee MYK, Bick DE, et al. (2015) A national survey of obstetric early warning surveys in the United Kingdom: five years on. Anaesthesia2014;69:687-9