Resources by experienced OB &
MFM physicians and L&D Nurses.
Are you a PeriGen Customer?
Join the PeriGen User Community
Highlighted Content
Explore more resources
Additional Information
Early Warning Systems
The Institute for Healthcare Improvement calls them “scorecards that save lives.” Originally created in answer to research finding that 40-50% of maternal deaths are potentially preventable, early warning systems seek to standardize clinical assessment and to facilitate recognition of maternity patients who have or are developing critical illness. Non-obstetric early warning systems have been use in Europe, especially Great Britain, for over twenty years. Systems adapted to obstetrics have started to gain traction in the US relatively recently.
There are two types of early warning systems. Single parameter systems rely on carefully defined threholds. Multiple parameters systems, often using weighted algorithms, result in a composite score that triggers protocol activities. Because most systems are manual, the type used is often a balance between practicality and clinical impact.
Following are links to published information on the design and use of obstetric early warning systems:
- Institute of Healthcare Improvements article “Improvement Stories: Early Warning Systems – Scorecards That Save Lives”
- “Use of Maternal Early Warning Trigger tool reduces maternal morbidity,” published in American Journal of Obstetrics & Gynecology
- “The Maternal Early Warning Criteria” from ACOG’s Obstetrics & Gynecology journal
- Royal Free Hospitals Clinical Guidelines for MEOWS in Maternity
- British Journal of Midwifery “A modified early obstetric warning system” reviews the use of a maternal early warning system at Kettering General Hospital
- ACOG’s recommended screening and review process for severe maternal morbidity
Other Reading:
- Design and Internal validation of an obstetric early warning score: secondary analysis of the Intensive Care National Audit and Research Centre Case Mix Programme database. (Anaethesia
- Saving Lives, Improving Mothers’ Care – Surveillance of maternal deaths in the UK 2011-13 and lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbitiy 2009-13 (National Perinatal Epidemiology Unit-MBRRAC-UK)
- Focus on Infants During Childbirth Leaves U.S. Moms in Danger (NPR)
This collection of resources provides guidance to L&D unit leads on providing consistent standards of care:
- NICHD Definitions & Classifications
- Issued in Feb., 2015 ACOG’s “Levels of Maternal Care” defines maternal care standards and nomenclature
- Northern New England Perinatal Quality Improvement Network (NNEPQN) guide to electronic fetal monitoring
- Regional Perinatal Programs of California’s compilation of perinatal standards
Use these resources to learn how organizations use best practices and benchmarking to improve performance.
- What is a best practice?
- How are best practices defined in health care?
- Patient safety & quality: A handbook for nurses
- Using the Journal Club to Teach & Assess Competence in Practice-Based Learning & Improvement
The following resources are helpful for those looking to incorporate unit and care management strategies others are using to improve key obstetric benchmarks.
- Journal of Midwifery & Women’s Care Journal: Best practices for second stage labor care (bearing down/positioning)
- Best Practices for Formal Mentoring Programs
- Idealized model of perinatal care (Institute for Healthcare Improvement)
The Category II Management App, a free web-based app (not-downloadable) offered exclusively by PeriGen, is based on published research and designed for US usage to help support the management of patients with FHR tracings in category II (present in over 80% of labors).
Only 4-8 clicks get you the suggested outcome and the app takes seconds to use.
- Answer a few questions about the tracing and labor status
- The application processes the data through the algorithm and presents its conclusion along with the publication’s original image.
This online app (not for download) can be used as often as needed on any computer or mobile device.
Register for the Category II Management App
(Before launching the web tool please read this important information.)
Any questions or feedback, email info@perigen.com
A Message from Thomas Garite, MD
Chief Medical Officer:

“Category II fetal heart rate tracings are common and cover a wide spectrum ranging from relatively minor findings to more significant combinations that require very different clinical management. This app based on a researched algorthm represents a practical set of management guidelines for clinicians to consider as they care for women in labor. The algorithm was designed in accordance with a fundamental premise in patient safety circles – that standardization and simplification of critical care processes promote better outcomes. Please do read the full publication that describes a number of important concepts that clinicians must also include in their clinical reasoning. No simple algorithm can handle every unusual circumstances or rapid change in the tracing. We look forward to your feedback and hope it will be a useful tool for clinicians to access on their smart phones when managing patients whose tracings are in Category II.”
“We present an algorithm for the management of category II FHR patterns that reflects a synthesis of available evidence and current scientific thought. Use of this algorithm represents one way for the clinician to comply with the standard of care, and may enhance our overall ability to define the benefits of intrapartum FHR monitoring.”
Reference Publication:
Intrapartum management of category II fetal heart rate tracings: towards standardization of care. Clark SL, Nageotte MP, Garite TJ, Freeman RK, Miller DA, Simpson KR, Belfort MA, Dildy GA, Parer JT, Berkowitz RL, D’Alton M, Rouse DJ, Gilstrap LC, Vintzileos AM, van Dorsten JP, Boehm FH, Miller LA, Hankins GD. Am J Obstet Gynecol. 2013 Aug;209(2):89-97. doi: 10.1016/j.ajog.2013.04.030. Epub 2013 Apr 27
http://www.ncbi.nlm.nih.gov/pubmed/23628263
When asked about their greatest challenges with existing EFM systems, labor & delivery clinicians consistently cite integration with their EHR. In keeping with Stephen Covey’s (Seven Habits of Highly Effective People) rule of “seek first to understand,” following are resources for understanding the mechanics and practices for integrating electronic fetal monitoring systems with major EHRs.
- HL7 — or Healthcare Language 7 — is a standard method of allowing systems to “talk” to each other. Here’s a HL7 101 primer that explains how.
- Biomedical Device Interfacing to Clinical Information Systems: A Primer, a fairly readable article by Bridget Moorman published in IT World in 2008.
- The National Learning Consortium’s Change Management in EHR Implementation provides a roadmap to continuously refining utilization of heatlhcare technology
- Dealing specifically with integrating EFM with major EHRs, PeriGen’s SVP of Product Management Bruno Bendavid outlines the challenges and potential solutions in his integration white paper and offers 10 tips for successful integration
The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) indicate that inadequate communications between providers or between providers and patients/families is the root cause of 60% to 70% of investigated sentinel events in medicine. When 47 perinatal deaths were investigated by JCAHO, poor communication was identified as the root cause in 72% of these adverse events.
One of the most common challenges experienced by labor & deliver management is maintaining efficient communications between team members, while consolidating a wide range of skill sets and personalities into a cohesive, effective unit. Here are a few information resources that may help you meet this challenge. Please feel free to suggest more.
- Benchmarking your communication process: A key part of the AHRQ Hospital Survey on Patient Safety focuses on communication process and offers a way to compare your performance in this area to your peers.
- The Institute of Healthcare Improvement offers an SBAR (Situation-Background-Assessment-Background) Toolkit
- The World Health Organizations guide to team building & communication training
- The authors of one of the all-time favorite management books, The Wisdom of Teams, offers a synopsis of their learnings on high performance teams here
- Complimentary access to Journal of Healthcare Information Management peer-reviewed article “Using Intelligent Electronic Fetal Monitoring to Reduce Iatrogenic Complications of Childbirth,” co-authored by Dr. Emily Hamilton, PeriGen’s Senior Vice President of Clinical Research
- Dr. Emily Hamilton summarizes two breakthrough studies related to reducing infant mortality in her PeriGen-exclusive article “What Have We Learned & Where are We Going?”
- ACOG’s December 2011 article Oxytocin for Induction, including Patient Safety Checklists
- MCN research article “Implementation of a System-Wide Policy for Labor Induction”
- Chapter of March of Dimes Labor & Delivery Clinical Handbook “Quality Improvement Opportunities in Intrapartum Care” by Steven Clark, Eric Knox, Kathleen Rice Simpson, and Gary D.V. Hankin (includes widely-used Oxytocin Checklist)
- Abstract summary from the American Journal of Maternal/Child Nursing “Patient Education to Reduce Elective Labor Inductions”
- Healthcare Informatics article “Elective Early Deliveries: One Hospital’s Groundbreaking Optimization Work”
- A new way to monitor the impact of interventions
- A Vision of the Future of Obstetrics, a free ebook authored by some of today’s perinatal thought leaders
- Building the perfect business case: Tips, tricks and templates
- MedCity News (Business of Innovation in Healthcare): A Final Four to Remember — and why it’s relevant to healthcare
- The Online Journal of Issues in Nursing: The Role of Buy-In in Bringing About Change
- Nursing Leadership Resources from the American Association of Nurse Assessment Coordination
- American Association of Nurse Executives provides Leadership Tools including benchmarks, inventories, and competency lists
- The Emerging Nurse Leader website lists a number of information resources for nurse leaders, many of them free. The site also hosts a blog
- AHRQ TeamSTEPPS Specialty Scenarios: L&D Leaders (these scenarios provide practice opportunities for defining and communicating processes to meet common L&D leadership challenges)
- Becker’s Hospital Review: Five ways automation can help reduce adverse events in labor & delivery
- Top Ten Skills of High-Performing Healthcare Leaders by B.E. Smith
- Ten Communication Secrets of Great Leaders, Forbes
Team-Building Tools & Tips
- The Science Behind Jeff Bezo’s Two-Pizza Team Rule
- Nine Team Building Activities developed for healthcare
- An oldie, but a goodie: Collaborative Healthcare Teams a Growing Success by Debra Woods
- Team Building Ideas for Hospital Workers (by Tony Ryan, Demand Media-Chron)
- Nursing Times: Effective team leadership: Techniques that nurses can use to improve teamworking
- Wikipedia article: Team nursing
- Achieving Strong Teamwork Practices in Hospital Labor & Delivery Units (Center for Military Health Policy Research)
The following information resources provide educational information on assessing labor progress, as well as the latest research on labor curves:
- Jun Zhang’s 2010 article on labor progress after 6 cm presents an update to the Friedman labor curve: Contemporary Patterns of Spontaneous Labor with Normal Neonatal Outcomes
- Royal College of Midwives discussion of the variables beyond dilation that help define labor progress: Evidence-Based Guidelines for Midwife-Led Care in Labor-Assessing Progress in Labour
- A research study in AJOG in 2013 finds that among those undergoing a primary cesarean because of failure to progress, 42.6% of primiparous and 33.5% of multiparous never progressed beyond 5 cm dilation
- Assessing first stage labor progression and its relationship to complications, authored by PeriGen’s Emily Hamilton MD and published in AJOG, provides a brief historical summary of progress assessment curves and presents an alternative method for measure progress before 6 cm
The following is a compilation of information resources providing practical, actionable strategies for fine-tuning your patient safety initiatives:
- Eight tools for improving obstetric patient safety and unit performance offered by Henry M. Lerner of Harvard Medical School on OBG Management blog
- Five best practices for high reliability in obstetrics as outlined by unit leaders from major US hospitals in 2016 ebook, The Future of Obstetrics.
- AJOG’s Patient Safety series article Perinatal High Reliability provides the key elements necessary for a successful patient safety initiative in obstetrics
- Dr. Williams Edwards Deming is considered by many to be the father of the continuous improvement movement. In this article, Five Deming Principles That Help Healthcare Process Improvement, Health Catalyst outlines how his core principles apply to healthcare
The Institute of Medicine defines protocols, or clinical guidelines, as “systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical situations.” The following information resources aim to help labor & delivery unit directors, chair people, and risk managers understand, leverage, and improve protocol compliance.
- The potential benefits & limitations of protocols
- An interview with Rebecca Steinfield, an IHI Improvement Advisor, with tips on improving your improvement program
- California Maternal Quality Care Collaborative’s tool kit for responding to maternal hemorrhage
- Outline and results research for a hemorrhage protocol (AJOG)
- The Institute for Healthcare Improvement’s evidence-based bundle for induction
- A common induction checklist
Shoulder Dystocia
Shoulder dystocia is typically defined as a vaginal birth where the baby’s shoulders get “stuck,” requiring extraordinary maneuvers to delivery the fetus. The incidence of shoulder dystocia varies based on fetal weight, maternal weight, and the presence of diabetes. Complications associated with shoulder dystocia include postpartum hemorrhage, maternal lacerations, and brachial plexus palsies.
- Abstract summary of “Outcomes associated with a structured prental counseling program for shoulder dystocia with brachial plexus injury”
- MD Advisor article co-authored by Dr. Emily Hamilton, SVP of Clinical Research for Perigen “Shoulder Dystocia, Neither Predictable nor Preventable, Not Anymore!”
The electronic fetal monitoring (EFM) resources below have been compiled from a review of materials readily available on the Internet. Although PeriGen is not responsible for the creation of this content — or for its continued availability and quality — they provide a comprehensive curriculum for clinicians seeking to gain a basic understanding of EFM. In addition to these EFM training resources, we’ve found several general, free online training resources of use:
- To start: A definition of electronic fetal monitoring
- The Basics of Electronic Fetal Monitoring (includes a history) by Emily Hamilton, MDCM
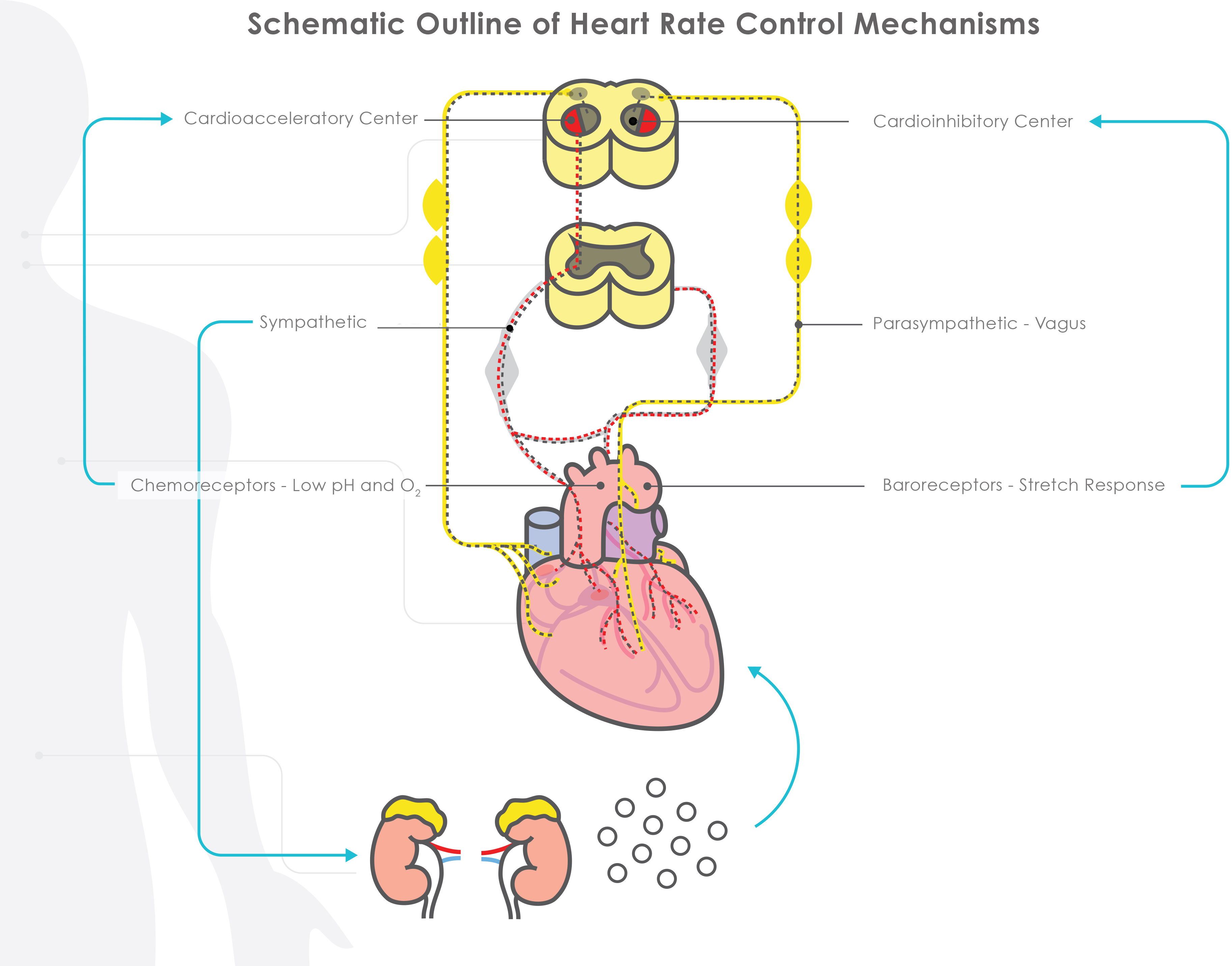
- The Physiology of the Fetal Heart Rate (an updated review of available research)
- The Future of EFM, an article summarizing current clinical & technology research that will impact electronic fetal monitoring
- ACOG’s EFM Training Toolkit (member log in required)
- Free study resource quiz
- EFM Education Certification programs offered by AWHONN
- The open-access EFM education credentialing examination offered by the Perinatal Quality Foundation
- A review of how current state-of-the-art EFM systems and perinatal analysis software work to support clinical care:
Electronic fetal monitoring definition:
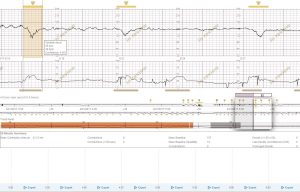
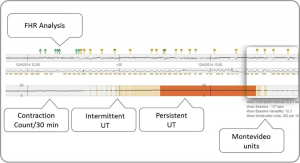
Electronic fetal monitoring or EFM is the practice of measuring and displaying fetal heart rate and contraction rate during labor. Traditionally, the output of EFM takes the form of tracings — a visual display of the fetal heart rate on top and the contraction rate on the bottom.
Like much technology, electronic fetal monitoring has progressed rapidly. The latest EFM software offers specialized displays so a detailed view of the tracing can be seen simultaneously with a longer term overview for trend analysis, pattern recognition, and color-coded notifications when specific combinations of EFM patterns are present. All of these advances help labor & delivery clinicians to spend less time on manual calculations, support improved care decisions, and better manage multiple patients.
This technology adds statistical analysis to the traditional EFM display to highlight abnormal patterns, yield meaningful summary information, and display the meaningful interaction between contractions and fetal heart rate via color-coded visual cues.
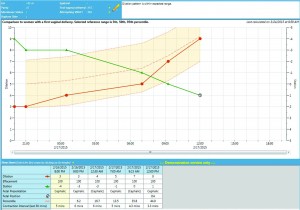
Some of the most recent technology adds an even greater depth of statistical interpretation to labor progress, comparing a single patient’s measurements to a large population of others sharing similar characteristics.
*PeriGen is approved by the California Board of Registered Nursing, Provider Number CEP16729. Video completion via a single computer/device per user is required for credit achievement. Once video completed, a web link is provided for completion of a mandatory course evaluation. Once evaluation is finished, an online certificate of completion is provided for printing and retention.
Workflow is defined as a set of tasks and resources need to accomplish to meet a goal. Defining and conforming to a set of processes enables a team to consistently achieve organizational objectives. Typical workflows in a labor & delivery unit include admission, documentation, and filling laboratory orders. Following are information resources on defining and optimizing workflows for labor & delivery teams.
- Organizational Workflow & its Impact on Work Quality (a chapter from Patient Safety & Quality: An Evidence-Based Handbook for Nurses)
- A review of realistically applying business process improvement practices to healthcare
- The “Integrating the Healthcare Enterprise” (IHE) technical framework for perinatal workflow delineates a standard process for each stage of L&D patient care
- Institute for Healthcare Improvement “IHI Perinatal Improvement Community” change package delineates a common set of process improvement goals and methods
- A case study highlighting the use of Lean Six Sigma to improve processes at a Maryland hospital
Following are items of broad interest to labor & delivery clinicians:
- Rebecca Cypher MSN PNNP reviews the research and results related to the use of technology in perinatal nursing in this white paper, “Technologies in Perinatal Nursing: Time to Accept & Embrace the Challenge.”
- IHI (Institute for Healthcare Improvement) Home Page for Maternal and Infant Health http://www.ihi.org/Topics/Maternal-Infant-Health/Pages/default.aspx
- AIM (Alliance for Innovation on Maternal Health) https://safehealthcareforeverywoman.org/
- AHRQ (Agency for HealthCare Research and Quality) Home Page for Maternal Care https://www.ahrq.gov/topics/maternal-care.html
- NICHD National Institute of Child Health & Human Development
- Safe to Sleep HomePage https://safetosleep.nichd.nih.gov/
- Child & Maternal Health Education Program https://www1.nichd.nih.gov/ncmhep/Pages/index.aspx
- Maternal Mortality Research Information https://www.nichd.nih.gov/health/topics/maternal-mortality/researchinfo