Reprinted from HISTalk, April 15, 2018 @ 9:41 am In Interviews
HISTalk Interviews Matt Sappern, CEO, PeriGen
Mr. HIStalk – Tell me about yourself and the company.
 I’ve been in healthcare IT for more than 15 years, holding various leadership roles across product development, services, support, and sales. Probably most formatively, I was at Eclipsys in the years leading up to its acquisition by Allscripts, and then I spent some time at Allscripts as well.
I’ve been in healthcare IT for more than 15 years, holding various leadership roles across product development, services, support, and sales. Probably most formatively, I was at Eclipsys in the years leading up to its acquisition by Allscripts, and then I spent some time at Allscripts as well.
PeriGen has been a remarkable learning opportunity for me over the past six years. PeriGen uses artificial intelligence to build nursing productivity tools, and more importantly, early warning tools for labor and delivery. All of these tools are embedded in PeriWatch, our comprehensive electronic fetal surveillance system, or EFM.
We’ve also just started to sell tools that work outside of the EFM of record so that hospitals don’t have to rip and replace their current system. I’ve heard too many department heads say, “I really need to use your analytics to provide better care, but we have to use Cerner’s system or we just signed a contract with another vendor before you got to us.” For those situations, we’ve developed PeriWatch Vigilance, an early warning system that works independently and provides the capacity for every nurse, every doc, every mother, and every baby to benefit from real-time analytics in labor without a costly rip-and-replace project.
What are the hot issues in labor and delivery?
The same chronic issues affecting all service lines. The rise of diabetes, hypertension, and obesity are extremely bad for the baby. Mothers are also getting older, which presents some complications as well.
At the same time, a lot of nurses are leaving the field. Phenomenally experienced baby boomer nurses are retiring. Young nurses have great levels of energy and great training, but they don’t have 10 years of experience and that developed gut to fall back on.
You have fewer OBs, less-experienced nurses, and nurses who are being asked to do quite a bit more relative to documentation and helping colleagues at the same time as you have a more complex maternal profile. It’s the perfect storm for trouble.
The US infant mortality rate is among the worst in the developed world, although the contributing factors are mostly social rather than medical. Have hospital advances made their care safer?
Well, we certainly have. We published a study along with MedStar where including our solution reduced unanticipated admissions to the NICU by about 50 percent. That’s pretty remarkable.
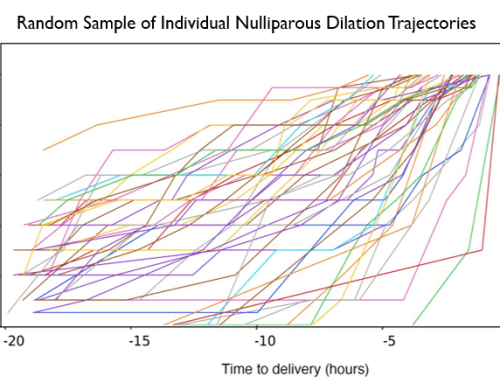
With bad outcomes in labor and delivery, it often comes down to the nurse not recognizing that there’s a problem on the strip. They don’t see the trends, they haven’t been trained, or they don’t have the equipment to see the long-term patterns. We show trending data, as opposed to, “In this second at this point in the day, there’s a fetal heart rate deceleration.” We’re showing the four-hour trend and a 12-hour trend, so the nurses get a more complete picture.
When you talk about reducing unanticipated NICU events by 50 percent, that’s remarkable. At MedStar, we took their medical malpractice payouts that were associated with OB from a full third of what they were paying in medical malpractice awards to — I think the last number I saw was in 2016 — about 8 percent, which is virtually unmatched by other hospitals in the country.
Unnecessary C-sections also affect outcomes and cost. Is that still a big issue?
C-sections are always going to be a heated debate. A lot of health systems have done a great job at managing the C-section rate, at least the low-hanging fruit where voluntary C-sections or planned C-sections have been reduced. You’re seeing a lot fewer planned C-sections for convenience, so that’s a good thing.
The trick is to not focus on too few or too many C-sections, but rather, “Have we made this decision with all the right data?” We’ve had hospitals use our solution to decide to not do a C-section and the mother had a successful vaginal birth 20 minutes later. It’s really a question of what data you have access to at that critical moment of judgment.
C-sections and labor progress for many years was focused purely on a linear time measurement. We’ve built tools that look at other issues. What’s the gestational age? Have they had a child before? Did they have an epidural? Have they had a C-section before? These are things you can do in real time with algorithms and artificial intelligence that can’t be done any other way.
Having worked with artificial intelligence, what are the lessons you’ve learned or your feelings about its place in healthcare?
It’s a very powerful tool that can be harnessed to help the clinician. There’s so much data that’s being generated. More and more monitoring is being done, both in the inpatient and outpatient world. But all of this data needs to be managed somehow. You need to take an approach of looking for exceptions in data. That’s what we use AI to do.
We use Google’s TensorFlow tools. We’re fairly advanced in how we use them. We work with a consortium of other Google users in Montreal, where we have a lab. As one builds algorithms, with machine learning, it is critical to teach these tools what they’re looking at and for. After that complex process, we lock down that algorithm and then build it into our application. We’re an FDA-cleared device, so we can’t have algorithms that are changing all the time.
We’ve taken a group of experts and used their review of many thousands of strips to teach the TensorFlow system what it needs to be looking for. We validated that, locked it down, and sent it through the FDA. It’s complex to use AI when you are working with software as a medical device.
What opportunities exist from having all of this data being collected electronically?
The challenge with data is its accuracy. Nurses, who generate a huge percentage of the data out there, are often challenged to be documenting exactly what should be documented at exactly the right time. Clinical settings are pretty crazy and they are always going to put the patient’s health above documenting, so there are inconsistencies in EMR documentation.
That’s just the nature of anything that is based on human input. There will always be levels of subjectivity. There will always be issues associated with time lag. That’s why we largely focus on data that’s being generated directly from medical devices.
That’s what makes our partnership with Qualcomm Life so interesting. They feel the same way. They bought Capsule and they’re focused on how to take information directly from medical devices and make it usable in real time. That’s what we do today. We’re the poster child for what Qualcomm Life is trying to do with Intelligent Care.
How does the Qualcomm relationship work?
PeriGen takes data directly from a device, digests it in real time, and serves it up to the clinician in a helpful manner to help them make decisions and monitor patients. That’s really what this relationship is all about. That’s what Qualcomm Life’s Intelligent Care platform is all about. Qualcomm looked at PeriGen and said, we need to be doing this across all service lines, both inpatient and outpatient.
We’re working with Qualcomm Life to think about what ambulatory devices in obstetrics can become. How data management in the ambulatory arena, how non-stress tests can be made more affordable, more frequent. Things that are going lead to better outcomes for premature babies as well. They’re a great partner. We think exactly alike and approach it from different and complementary strengths.
How can clinicians monitor that huge amount of data?
It’s a big issue. More often than not copious data becomes a tremendous distraction. It’s not only the amount of data, but the quality of data. The degree of human intervention is directly related to the degree of inaccuracy that you’re going to have in this data.
Better to take the data directly from devices, perform real-time analytics on it, and present it up to the clinician to help their view of what’s going on with the patient. Not to tell the doctor what’s happening to this patient and certainly not to tell the doc what to do to this patient, but to serve it up to the doctor and nurse as, “This is what we are seeing. Your health system has asked you to consider something when this is going on.”
When we started working with HCA, they said, “We have developed some of the most remarkable safety protocols for managing oxytocin and other things. How do we help the nurses in a clinical setting on the floor take advantage of these protocols? When a patient starts exhibiting non-reassuring signs, how do we make sure that we’re getting to that patient in a timely fashion across the board in a standardized way? How do we automate our checklists?”
That’s what PeriGen does. Nurses and docs know how to care for patients in certain conditions. We’re just trying to make sure that they understand and see those conditions coming much more frequently, more consistently, and in a more standardized fashion.
Is there overlap with what EHR vendors are doing with their products?
We’re quite complementary to what most of the EMR vendors are doing. We’re not about documentation and that’s their strong suit. Epic, Cerner, Allscripts, and Meditech manage an awful lot of data. They are looking at ways that they can create specific alerts and reports from the data and create telemedicine monitoring capability. I applaud that. Those are all things that must happen in healthcare.
We’re doing the same thing. We’ve created a telemedicine platform that allows a single clinician to look out over 10, 12, or 20 hospitals and intervene on only the cases that are starting to show non-reassuring trends. The difference is that the EMR vendors are using EMR data, which is meaningful, but often subjective, and the timing is somewhat subjective as well. We’re taking information directly from the medical device in real time.
I think there’s a great alchemy there. We have clients using Epic’s tools for telemedicine in unison with some of the tools that we provide. They seem happy having access to both. It’s sort of a left and a right side of the brain effect.
We continue to roll out our telemedicine functionality at Ochsner. Just about every client and prospect we’re talking to right now is interested in our telemedicine hub, which allows a single clinician to look out over multiple labors and determine if there’s something out of the norm that needs intervention. Some of our clients want to make a business out of it, where they provide an over-watch service for community hospitals in their regional area. Some will use it with a single individual who provides great clinical leverage across the entire health system.
Do you have any final thoughts?
My hope is that a lot of other companies start doing what PeriGen is doing in terms of managing data and making it meaningful. We can’t lose sight of the fact that improved and distributed capability for monitoring patients generates more and more data that has to be managed by fewer and fewer clinicians. There will continue to be a reliance on tools like PeriGen’s to separate the wheat from the chaff. What do I have to tackle immediately and intervene before it gets tough?
I would challenge the rest of the industry to be looking for ways to employ artificial intelligence and other types of algorithmic approaches to managing data. It’s just overwhelming for clinicians at this point.
Read the original article on HIStalk by clicking here